Vaccine Update
There’s another vaccine progressing toward emergency use authorization, from Oxford-AstraZeneca. This vaccine technology is different than the mRNA vaccines from Pfizer and Moderna. Instead, it uses an adenovirus that has been engineered to carry a copy of the SARS-CoV-2 spike protein gene. Adenoviruses are a family of viruses, many of which cause the common cold. In this situation, the adenovirus serves as a delivery vehicle to bring the spike protein gene to the place where it will be processed by the human cell - the nucleus. The adenovirus itself is not able to replicate inside of the human cell, so it will not cause an infection in vaccine recipients. It literally is a delivery vehicle. I thought the New York Times made a great visualization of how this vaccine works.
Interim analysis of AstraZeneca vaccine indicates it is an efficacy of 70.4% but recent comments by the CEO of AstraZeneca suggest that the efficacy might be higher. Remember, science doesn’t make decisions by taking CEOs at their word or based on press releases. Instead, science and health policy is based on peer-reviewed data. So we’ll see what comes of the FDA’s analysis of the vaccine as it continues through the process. You may recall that the Pfizer and Moderna vaccines have an efficacy of ~95%, meaning that they prevent illness in 95% of vaccine recipients. That the AstraZeneca one is potentially less efficacious is offset by a very important tradeoff - it is made of DNA, not RNA, so it is a much more stable molecule that can be stored at refrigerator temperature for up to 6 months. This will be a very important vaccine, indeed, for vaccinating the developing world and rural areas where (ultracold) freezers might not be widely available. The US has entered into a contract with AstraZeneca for 300 million doses of their vaccine as part of Operation Warp Speed.
Post-Christmas Reminders
If you gathered for Christmas, please assume that you were infected at your gathering and self-quarantine for 14 days following the event. You can seek out a test about 7 days after, so this coming Saturday. I hope you had a marvelous time at your gathering, really and truly. Self-quarantine is the consequence of that choice, however. For my readers who are >65 or who have underlying medical conditions, consider sheltering in place this week and next. The people who gather for Christmas and New Years, ignoring public health advice, will be infectious and in the community during these weeks. Be safe.
The data will be weird for probably the next two weeks due to back to back holiday closures and reporting delays. Kansas, in particular, did not report any data on Friday and we might expect the same thing this week.
The World
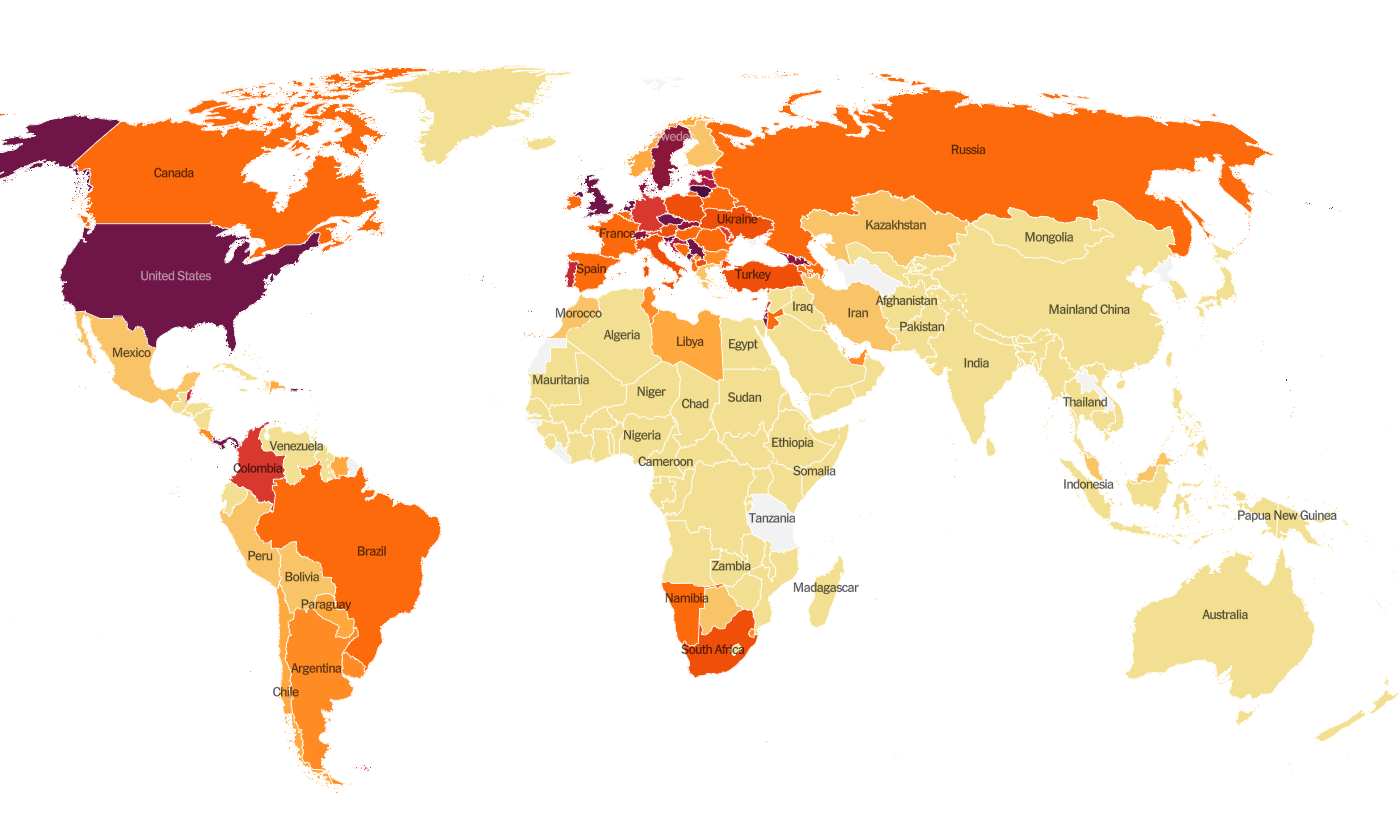
Globally, the SARS-CoV-2 virus that causes COVID-19 disease has sickened >81.1 million people (+4.2 million since last week) and killed at least 1,769,400 (+74,700 in the past week) as of this morning.
The US is ranked in the second highest color category for hot spots. We are ranked #9 in the world for average daily case rate per 100,000 people over the past 7 days (last week, 12th) with a rate of 55.7 compared to 65.1 last week. So our case rate is getting better. But case rate is improving even more dramatically for other nations, causing our ranking to climb up. The top five countries for average daily case rate per 100,000 in the past week are Gibraltar, Liechtenstein, Lithuania, Panama and Montenegro.
For deaths, the US average daily death rate per 100,000 over the past week is 0.7 (previous week was 0.8), and we are ranked #23 in the world for this (last week we were ranked #21). The top five countries for average daily death rate per 100,000 in the most recent week are Liechtenstein, Croatia, Slovenia, Bosnia and Herzegovina, and Hungary.
The United States
As of this morning, there have been over 19.2 million cases (+1.4 million in the past week) and 317,800 deaths in the US (+16,330 in past week). Keep in mind that both of these numbers are probably an under-count of the situation in our country.
This week we see things have gotten better for much of the Midwest, the Pacific Northwest, upper plains states and the Rocky Mountain states of Colorado, Wyoming and Montana. There is still a swath of more intense disease rate from Illinois to Pennsylvania. And, of course, things continue to be intense along the southern half of the United States. We should remember that some of this improvement may be an artifact of delayed reporting over the holiday. The top five states in the nation for average daily case rate in the past 7 days are California, Tennessee, Arizona, Alabama, and West Virginia. Oklahoma, our neighbor to the south, is ranked #6. The top five states in the nation for average daily death rate in the past 7 days are South Dakota, New Mexico, Pennsylvania, Arkansas and Rhode Island.
There’s a new data resource available to us now from the federal government, called the COVID-19 Community Profile Report and it is a TREASURE TROVE of data for counties and cities. It is formatted in much the same way as the White House Coronavirus Task Force reports but with one key difference - this resource DOES include Georgia’s antigen cases in their total whereas the WHCTF does not. So this resource is the best head to head comparison we have for how Georgia is faring relative to other states. There is both a PDF and an excel file (this is the gold mine of data) of the report at the link above that you can download and review. They break the US into FEMA regions and you can find how your state is classified here. My Georgia readers are in region 4. Kansas readers are in region 7. The first map I want to bring up from the Community Profile Report from 26Dec2020 is this one that shows how case rate per 100,000 is increasing or decreasing across the country. Most of Kansas is colored green, meaning a big drop in case rate per 100,000 last week. This is good news.
Next let’s look at the map below of rapid riser counties. What you’ll notice is that the middle of the country is largely blank here. The upper Midwest and northern Plains states are relatively quiet, things are holding steady or decreasing. Instead, the counties of concern are the coastal states and sunbelt. There are, however, a handful of counties in Kansas that are considered rapid risers.
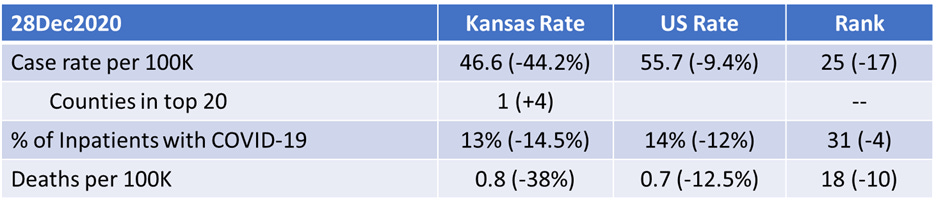
The table below tells you where we are this week and how that compares to the previous week (in parentheses). The data for everything but the percent of inpatients with COVID-19 comes from the New York Times coronavirus tracker and is current as of this morning. The hospital data comes from the HHS Community Profile Report from 26Dec2020. Keep in mind that some states did not report data over the holiday, so the rankings might not be accurate assessments of how states compare this week.
Kansas has been dropping across all the metrics here. Again, some of this decrease may be an artifact, but probably not all of it. Our new case rate per 100,000 is now less than the national average and so is our patient census (the percent of hospital inpatients who are being treated for COVID-19). The one area where we gained was one county that is in the top 20 for new case rate, Pawnee county.
Next, let’s look at how seasonal influenza is impacting different states across the US. You can consult FluView any time you’d like to see this map and other data visualizations. You can read the weekly report from Kansas Department of Public Health here. The maps below show last year’s map for the 51st week of the year (left side) and this year’s map for the same week on the right side.
The entire country remains in the minimal zone for influenza. Compare that to where we were a year ago for week 51 in the map on the left. The things we’re doing to limit the transmission of COVID-19 are also interrupting the transmission of influenza. Of course, COVID-19 is more transmissible than influenza so we aren’t seeing the same impact for COVID-19. But it’s a pretty great way to see what is possible through collective effort. Imagine a map that looked like this for COVID-19 if we could get more people to wear a mask. Remember, it’s not too late to get your flu shot. Please do so, if you haven’t already.
Kansas
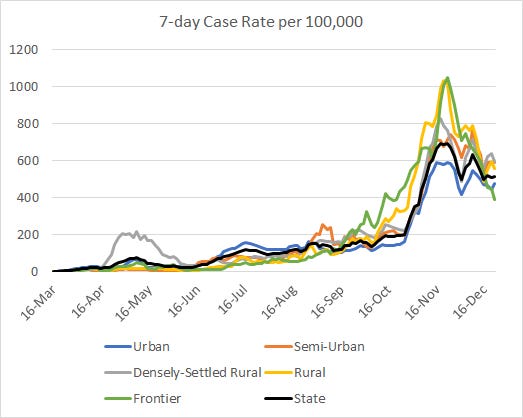
There is a vast improvement for Kansas this week when we look at county by county risk levels using this tool from the Brown University School of Public Health, last updated 24Dec. Whereas last week there were only two green counties and three orange ones, this week there are 14 green counties, 6 that are yellow, and 26 in the orange zone. Several of our most populated counties are in the red zone. If you’ll remember, the western half of the state is where the fall/winter surge really began for Kansas. So seeing that side of the state doing better is a good sign.
Case rate per 100,000 residents is trending down over the past month. From experience watching surges in other states, I can tell you that it takes a lot longer to come down from a surge than it did to reach the peak. So our work is not yet finished and we need to continue to be vigilant with mask wear, social distancing and hand and cough hygiene. However, we were still experiencing a high rate of disease as we headed into Christmas. So if a lot of people gathered as they have in the past, we might experience a resurgence of disease. When there’s this much disease in the community, momentum can shift very fast.
We still haven’t yet seen a peak for this surge when it comes to the death rate. There has been a lot of noisy variation in the statewide death rate for much of December, so I’m not convinced that the most recent downturn is real yet. With time we will gain needed perspective. The statewide death rate is about 10 times higher than where it was on September 1st.
The graph below shows the total test output (blue line, corresponds with left y-axis) and the total number of positive tests (gray line, right y-axis) over time. Note that the two y-axes do not have the same scale. Leading up to Thanksgiving, we had a lot of positive tests that remained high, regardless of test output. Since the first week of December, though, the number of positive tests has been declining. This is good news. But you’ll notice a weird change in the pattern of the data recently. Instead of seeing this weekly peak followed by a weekend decline, we see this continued dropoff after 24Dec. The same thing happened at Thanksgiving (see the trend around 26Nov). This is holiday/weekend effect. It makes it harder to see where we really are. All the same, it is good to see the percent positive rate coming down.
The graph below shows how many clusters of COVID-19 disease have been associated with various settings over the past 8 weeks. You’re looking at 8-week timelines, side by side. What we can see is that long term care facilities (LTCFs) remain the largest source of outbreaks, which is why these residents and staff are near the front of the line for the COVID-19 vaccines. A second tier of settings with similar counts of outbreaks are private businesses, private events and schools. As a reminder, just because a business, event or school says you don’t have to wear a mask on the property doesn’t mean it is safe to not wear a mask. Or observe social distancing.
According to the New York Times coronavirus vaccine tracker, Kansas has been allocated 130,450 vaccine doses as of 28Dec. And at least 24,000 have arrived in the state. Of those doses received, 600 have been administered, or 2.5% of the doses on hand. The Pfizer doses are being administered to LTCF residents and staff through a partnership between CDC and CVS and Walgreens. The Moderna vaccines are being distributed to healthcare workers as of the 22Dec Kansas vaccine update. A similar update might be provided tomorrow.
A reminder, Operation Warp Speed only covered the development, manufacture and shipment of the vaccines to the states. The “last mile” of transforming a vaccine into vaccinations is the responsibility of the state. And many states have dramatically cut public health funding for the past decade. They are also feeling the financial strain of the pandemic. So there isn’t a lot of money to move around to various needs. There likely isn’t the funding nor the infrastructure to support a statewide vaccination roll out at the speed that any of us would see as reasonable. The coronavirus relief bill that was signed into law late last night includes 8 billion dollars for vaccine distribution, but we don’t yet know how that money will be allocated to the states. So if you are growing impatient about the speed with which the vaccine is being distributed, perhaps get in touch with your state senators and representatives as well as your representatives and senators in Congress to ask for better funding for public health. Nothing in this country happens for free.
There are 2.9 million residents in Kansas, so we have a long way to go. In the meantime, the nonpharmaceutical interventions such as wearing a mask, social distancing and good hand and cough hygiene are going to be the best protection we have against the virus. So keep doing those things. Help is coming, but it is slow.
References
https://www.coronavirus.kdheks.gov/160/COVID-19-in-Kansas
https://www.nytimes.com/interactive/2020/world/coronavirus-maps.html
https://www.cdc.gov/flu/weekly/fluviewinteractive.htm
https://beta.healthdata.gov/National/COVID-19-Community-Profile-Report/gqxm-d9w9
https://www.fema.gov/about/organization/regions
https://www.nytimes.com/interactive/2020/health/oxford-astrazeneca-covid-19-vaccine.html
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)32661-1/fulltext
https://www.hhs.gov/coronavirus/explaining-operation-warp-speed/index.html
https://www.nytimes.com/interactive/2020/us/covid-19-vaccine-doses.html?action=click&state=default®ion=hub&context=storyline_vaccine_hub&module=styln-coronavirus-vaccines&variant=show&pgtype=LegacyCollection
https://www.coronavirus.kdheks.gov/DocumentCenter/View/1696/COVID-19-Vaccine-Updates-12222020-
Kansas COVID-19 Updates is a free newsletter that depends on reader support. If you wish to subscribe please click the link below. There are free and paid options available.
My Ph.D. is in Medical Microbiology and Immunology. I've worked at places like Creighton University, the Centers for Disease Control & Prevention and Mercer University School of Medicine. All thoughts are my professional opinion and should not be considered medical advice.