Vaccine Update
Kansas is ranked #22 in the nation in terms of vaccine doses distributed to the state per 100,000 by the federal government (last week #46), and #46 in terms of persons receiving at least 1 dose per 100,000 residents (last week #37). In terms of the percent of the population who has received at least one dose, Kansas is ranked #45. The state has used 43% of its dose allocation, ranking it #48 in the nation. What does all of this mean? It means that we have fallen off the pace for getting vaccinations to the people who need them. We’re in the top half of the states in terms of getting doses from the federal government, but we aren’t using them efficiently and are near the bottom for using the precious doses we’ve been given. It’s really not okay. Those doses represent lives saved (or not saved).
You can see the Kansas vaccine information page here. The Centers for Disease Control and Prevention COVID-19 Vaccine Data Tracker is also a useful too, but be advised that the Kansas numbers are only updated with them on Monday, Wednesday and Friday.
I do want to point out some news from Merck, a vaccine manufacturer (with a long, successful history in vaccine development) that was developing two candidate COVID-19 vaccines. Three days ago, they decided to discontinue their studies because the vaccine candidates did not show adequate efficacy (i.e. preventing disease) compared to natural infection or the already EUA-licensed vaccines (Pfizer and Moderna). This matters for two reasons: (1) it’s a reminder that we are VERY lucky to have two vaccines with ~95% efficacy; (2) it might provide reassurance to many that the vetting process for the COVID-19 vaccines is thoughtful and robust. Vaccines that don’t work or that have intolerable side effects do not advance through clinical trials and the FDA approval process. The fact that the Pfizer and Moderna vaccines did make it through these trials and approval process is a big deal.
It does appear that the White House Coronavirus Task Force (WHCTF) reports will continue and today the Biden administration released the reports for all 50 states and US territories. This is a really big deal. I can’t tell you how many open records requests I’ve had to file for multiple states in the past year for these reports. Many states were responsive to my requests (including Kansas) but a good chunk of them were not. In July, I requested the 50 States reports from the Department of Health and Human Services (Secretary Alex Azar was the chair of the WHCTF) and the FOIA request remains unanswered, six months later. And yet, these reports included important safety recommendations for the population. Not every state has had the funding for robust data dashboards. These reports were an important equalizer and it was deeply troubling and unfortunate that the American people didn’t have equitable access to COVID-19 data and safety recommendations. I’ll be peppering in data throughout today’s report that compares Kansas to the US rate for various metrics, from these WHCTF reports.
Combined Data
The graph below shows us how some of our most important data points are moving over time. Cases are represented by the blue line and correspond with the left y-axis. All other metrics (hospitalizations, ICU admissions, deaths) correspond with the right y-axis.
Cases, hospitalizations and deaths are all dropping dramatically. That’s a good thing. But ICU admissions continue to hold steady at a high level.
According to the most recent WHCTF report, Kansas has the following rankings:
#24 for new cases per 100,000
#27 for test positivity
#28 for new COVID-19 hospital admissions per 100 beds
#39 for new deaths per 100,000
Testing
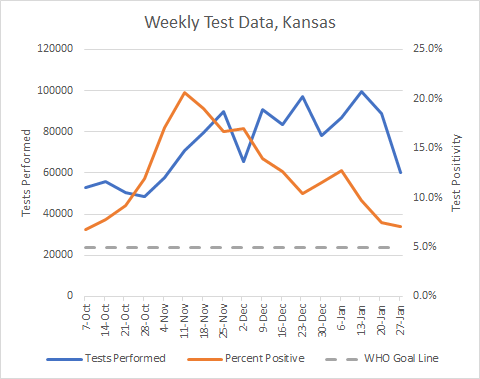
The graph below shows us how Kansas is doing for tests performed (blue line, left y-axis) and the percent of those tests that are positive (red line, right y-axis) on a weekly basis. The goal line for test positivity (5%) is indicated by the gray, dashed line.
Test output has declined 39.4% in the past two weeks. This is really, really concerning because while cases are declining they remain really high. In addition, the arrival of the more transmissible variant from the United Kingdom (known as the B.1.1.7 variant) has been found in several states (315 cases so far) and often these people don’t have a history of recent travel. That suggests that the variant has been spreading quietly throughout the country. The idea that Kansas has 0 reported cases so far does not mean it’s not here already. The US does not have a robust surveillance program to watch for this variant. We likely have many, many more of these cases than we realize. This variant is expected to result in a dramatic rise in cases. When I see the test output drop as it is here, then I worry that we will have a dramatic rise in cases (especially asymptomatic ones) that we can’t see or detect. It might make it harder for hospitals to see what’s coming. But we will see the impacts on hospital burden and death.
The percent of tests that are positive has continued to decline, but at a slower rate than before. The most recent week’s positivity rate was 7.1%. So we’re still above the 5% goal line, but the rate is decreasing. Test positivity is helpful for telling us if we are doing enough testing. The idea is that we want 95% of the tests we perform to be negative - it’s an indication that we are testing widely enough to not miss many cases. The higher the positivity rate, the more cases we are likely missing and those missed cases contribute to ongoing disease transmission in the community. The higher the positivity rate, the more likely our current case count is an underrepresentation of the disease burden.
Cases
In the past week there have been 9,105 cases newly reported by the Kansas Department of Health and Environment. That’s a decrease of 20% compared to the previous week. The weekly case rate per 100,000 residents is tracking along with the national rate over the past month.
The state average has decreased from the peak experienced in mid-November, and has declined sharply in the past two weeks. That means things are getting better but there is still a LOT of disease in the community. In fact, the current 7-day case rate is 60% higher than where we were prior to the fall/winter surge. That’s a vulnerable place to be, because that means there’s a lot of disease that could drive further increases given the right conditions.
The map below comes from the Brown School of Public Health. It grades each county’s level of risk, based on the average daily cases per 100,000 over the most recent 7 days. Risk is greatest for red counties and least for green counties. A month ago, the entire state was red. Now, we see definite signs of improvement, especially for the western half of the state.
Next, let’s look at where the most recent week’s cases are coming from in terms of age groups. The graph below shows 8 week timelines for each age group with the most recent week shown in maroon. One heads up, the “week” of 19-23Dec was a shorter week than usual so that week’s data are an anomaly.
This week we see continued decreases for every age group. That’s certainly good news.
Hospitalizations
This week there were 332 newly reported hospital admissions compared to the week prior, a decrease of 15%. The graph below shows us where those hospital admissions are coming from in terms of age group, over the past 8 weeks. I want to again remind you to not worry too much about the week of 19-23Dec because it was a short week.
Many age groups saw a decrease this week. But increases were noted for those 10-34, and 55-64.
An important question is how hospitals are coping with the burden of COVID-19 and one way to measure that is how COVID-19 patients compare to their overall patient load (sometimes referred to as the patient census). Among the most critical resources for severe cases of COVID-19 are ICU beds and ventilators and the staff that support those resources. The COVID-19 burden for both of these resources has been elevated but stable for the period between 15Nov and the start of the new year. The COVID-19 patient census for both ICU beds and ventilators has decreased since the start of the new year and hopefully that trend continues.
According to the HHS Community Profile Report for 26Jan2021, Kansas is ranked #30 in the nation for new COVID-19 admissions per 100 beds (last week #28). This is the same source of data that’s used for the White House Coronavirus Task Force reports, but updated daily rather than weekly. The report also indicates that 59% of the state’s inventory of inpatient beds are occupied (within normal limits) and 10% of the state’s beds are being used by COVID-19 patients (yellow zone). If we look just at the state’s ICU beds, then 77% of them are full (normal) and 23% are occupied by COVID-19 patients (red zone).
Deaths
Using the HHS Community Profile Report (date 26Jan2021), Kansas has the 41st highest newly reported death rate per 100,000 residents in the country, a huge drop from where we were last week (6th).
In the most recent week, Kansas has reported a net increase of 143 deaths, a decrease of 35% compared to the previous week. The graph below shows us how deaths have trended over time, adjusted for each county type’s population size. The statewide average is shown in the black line. You can check your county’s classification here.
The death rate for Kansas dropped like a stone, which is really strange actually. It makes me wonder if we have some delayed reporting going on because typically it takes a lot longer to descend from a surge than to climb it.
We can also see where deaths are coming from in terms of age group in the graph below. Like the other demographic graphs, this shows 8-week timelines for each age group. This week we saw decreases for all age groups.
Schools
I’ve been asked multiple times to weigh in on arguments for and against in person instruction in the K-12 setting. I have been reluctant to engage in local disputes but you are all welcome to use the data that I provide to make your arguments. Another reason for my reluctance is conflicting information. Case rates appear to be lower among children than other age groups. But we also know that we aren’t really looking for disease in children. Children have the highest test positivity rate (see green line in the graph below), meaning that we aren’t testing them widely enough and it’s not even close to the positivity rate for other age groups, especially in the fall/winter surge.
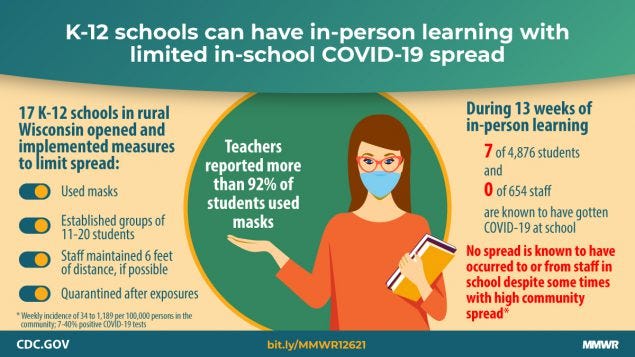
Yesterday the CDC publicized a study with the graphic below that demonstrated that having a strong safety culture in the K-12 setting resulted in very limited disease transmission in schools. They also wrote a “viewpoint” article in the Journal of the American Medical Association, akin to an op-ed in academic and medical journals.
I’m going to highlight two paragraphs from the viewpoint article and then wrap up with my thoughts:
However, the preponderance of available evidence from the fall school semester has been reassuring insofar as the type of rapid spread that was frequently observed in congregate living facilities or high-density worksites has not been reported in education settings in schools. Preventing transmission in school settings will require addressing and reducing levels of transmission in the surrounding communities through policies to interrupt transmission (eg, restrictions on indoor dining at restaurants). In addition, all recommended mitigation measures in schools must continue: requiring universal face mask use, increasing physical distance by dedensifying classrooms and common areas, using hybrid attendance models when needed to limit the total number of contacts and prevent crowding, increasing room air ventilation, and expanding screening testing to rapidly identify and isolate asymptomatic infected individuals. Staff and students should continue to have options for online education, particularly those at increased risk of severe illness or death if infected with SARS-CoV-2.
And the second paragraph:
Decisions made today can help ensure safe operation of schools and provide critical services to children and adolescents in the US. Some of these decisions may be difficult. They include a commitment to implement community-based policies that reduce transmission when SARS-CoV-2 incidence is high (eg, by restricting indoor dining at restaurants), and school-based policies to postpone school-related activities that can increase risk of in-school transmission (eg, indoor sports practice or competition). With 2 vaccines now being distributed under Emergency Use Authorizations and more vaccine options anticipated to be available in the coming months, there is much hope on the horizon for a safer environment for schools and school-related athletic activities during the 2021/22 school year. Committing today to policies that prevent SARS-CoV-2 transmission in communities and in schools will help ensure the future social and academic welfare of all students and their education.
So here are my thoughts. Yes, we can reopen K-12 schools safely but that depends on schools and the surrounding community committing to having a strong safety culture. Unfortunately, I think that there are too many school districts and the surrounding communities that have NOT adopted a strong safety culture (i.e. masks are optional among other problems). I’ve seen the pictures of crowded hallways filled with maskless students. I’ve seen the pictures of full gymnasiums to watch a basketball game where no one in the building is wearing a mask.
We cannot live life as we did prior to the pandemic, not yet anyway. We cannot have our cake and eat it too. We need to prioritize the things that are most important. If it is vitally important for a local community to have indoor dining options (for the economic survival of the community, for example), then that’s not sustainable with safely offering face to face instruction. If indoor high contact sports are important, then perhaps it’s best for those children to attend school virtually, or postpone/cancel indoor sports until disease rates decline with the vaccination.
References
https://covid.cdc.gov/covid-data-tracker/#vaccinations
https://www.kansasvaccine.gov/
http://www.ipsr.ku.edu/ksdata/ksah/population/popden2.pdf
WHCTF report repository: https://beta.healthdata.gov/browse
https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/index.html
https://www.cdc.gov/mmwr/volumes/70/wr/mm7004e3.htm?s_cid=mm7004e3_w
https://jamanetwork.com/journals/jama/fullarticle/2775875
https://beta.healthdata.gov/National/COVID-19-Community-Profile-Report/gqxm-d9w9
Kansas COVID-19 Updates is a free newsletter that depends on reader support. If you wish to subscribe please click the link below. There are free and paid options available.
My Ph.D. is in Medical Microbiology and Immunology. I've worked at places like Creighton University, the Centers for Disease Control & Prevention and Mercer University School of Medicine. All thoughts are my professional opinion and should not be considered medical advice.