Marking one year of COVID-19
According to the Kansas Department of Health and Environment, the first COVID-19 cases in the state of Georgia were reported on 09Mar2020. As we go through this month, there will be a lot of reflection of the successes and failures of the past year.
But my initial bit of reflection as I think back on the past year is how incredibly lucky we are that the virus that caused this pandemic wasn’t more contagious or more lethal than it is. As a reminder, coronaviruses are a large family of viruses that cause human disease that spans in severity from the common cold to the SARS virus that swept through Asia in 2002 - 2004 and the MERS virus that appeared in the Middle East in 2012. The MERS virus was less transmissible, but far more deadly than COVID-19. The SARS virus was as transmissible if not slightly more transmissible than COVID-19 and more fatal. For those who are unfamiliar, R0 (pronounced “arr-not”) is the basic reproduction number of the disease, or how many people one sick person is likely to infect, on average. It’s one way to compare the transmissibility of viruses or how contagious they are.
We are lucky because our state and our country clearly demonstrated that our public health infrastructure was not ready for a pandemic. There were challenges with leadership openly conflicting with public health experts that didn’t help the situation, to be sure. But decades of stripping public health budgets at the local, state and federal levels caught up to us in a big way. We also never saw public buy-in to public health guidance as leaders deferred responsibility for containing the pandemic down to individuals (a lost cause because pandemic response requires coordinated action) and the pandemic was heavily politicized. Without a clear and consistent message, people broke into factions that either saw the pandemic as a threat or saw it as a hoax.
Even now, a year and more than 500,000 deaths later, many of us in public health are sounding the warnings that we are seeing signs that cases may be rebounding nationally and regionally. Yet it is clear that the public is DONE with this pandemic. The vaccine is here and that is definitely the light at the end of the tunnel. But we are seeing governments ease up on restrictions and people relaxing their own disease prevention strategies, assuming we are closer to herd immunity than we actually are. It is nothing short of a miracle that scientists were able to identify the SARS-CoV-2 virus, sequence it and generate not just one but three safe and effective vaccines in a year. But with cases possibly rebounding, more transmissible variants emerging, and pandemic fatigue looming large, we aren’t deploying the vaccine fast enough and especially not in Kansas. So again, although we mourn more than 500,000 dead from this virus, we are lucky that it wasn’t worse. We could be talking about 2.8 million dead as of this week if it had been SARS. I say this not to discount the unimaginable suffering of those who have lost loved ones or who suffered the disease themselves. I say it to remind us that the work here is not finished and we remain a long way off from herd immunity. We weren’t ready for this pandemic, clearly. Let’s do the work to ensure we are ready for the next one.
Vaccine Update
Kansas is ranked #46 in the nation in terms of doses administered per 100,000 residents (last week #42). According to NPR, 14.8% of the Kansas population has received at least one dose of the vaccine and 7.2% of the population has received 2 doses. For reference, the national average is that 15.9% of the population has received at least one dose and the leader is Alaska, with 23.3% of its population vaccinated with at least one dose. Kansas has used 64% of its dose supply, ranking it #50 in the nation. What does all of this mean? It means that Kansas has a lot of room for improvement in its vaccination effort. Doses are limited across the country, of course. However, the state needs to be doing more to organize and administer the vaccines it *does* have available. The state has 359,144 doses on hand, sitting in freezers. Vaccines can’t save lives when they’re in a freezer. The supply problems that were a problem in the early stages of the vaccine rollout have been remedied as manufacturers have been able to accelerate production. In addition, the federal government is now able to give states a 3 week heads up of how many doses are coming and when. So there’s really no need to hang on to this big of an inventory. At most, the state needs to hold on to a few days worth of doses because more and more doses are coming every day.
You can see the Kansas vaccine information page here. The Centers for Disease Control and Prevention COVID-19 Vaccine Data Tracker is also a useful too, but be advised that the Kansas numbers are only updated with them on Monday, Wednesday and Friday.
But vaccine administration isn’t the only challenge to reaching herd immunity. At last weekend’s ACIP meeting they discussed the new Johnson and Johnson vaccine. But in one of their presentations they also brought up this survey that was done by the US Census Bureau that asked people who had not yet received a COVID-19 vaccine whether they would definitely get one once it was made available to them. Nationally, 54.5% of those who haven’t yet received a vaccine said they would definitely get one. The leader was Vermont, with 69.9%. Hey that number is pretty close to 70%, the herd immunity threshold, wink, wink. The Kansas percentage was 57.4%. Vermont is going to have a much easier time reaching herd immunity than Kansas will. But at least Kansas is above the national average. We will get there.
I’ve done another edition of Vaccine Q&A, with a deep dive on the Johnson and Johnson vaccine clinical trial data, as well as answering questions about vaccines and fertility/pregnancy/lactation, and what you can do after vaccination.
The most recent White House state report on Kansas was made public yesterday and is generated on Sundays. So the data are already a little out of date. But it helps us to see how Kansas is doing relative to the nation.
Kansas has the following rankings within the US. All of these are big improvements over the previous week’s numbers.
#40 for new case rate per 100,000 (orange zone)
#28 for test positivity (light green zone)
#28 for new hospital admissions per 100 beds for COVID-19 (yellow zone)
#17 for new deaths per 100,000 (light red zone)
Combined Data
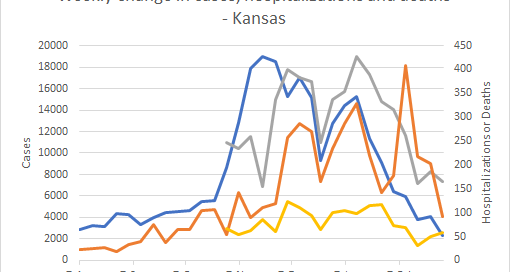
The graph below shows us how some of our most important data points are moving over time using data provided by the Kansas Department of Health and Environment. Cases are represented by the blue line and correspond with the left y-axis. All other metrics (hospitalizations, ICU admissions, deaths) correspond with the right y-axis.
Cases continue to decrease and the state is well below the pre-fall surge baseline. Hospital admissions and deaths both decreased this week too. ICU admissions increased over the past week, for the second week in a row.
Overall, Kansas seems to be in a much better position than it was in November and December. However, the more transmissible variant that rose to dominance in the United Kingdom is now present in Kansas, and likely widespread. Even though things are trending down right now, it’s important to continue to adhere to public health guidance so that we can prevent a renewed surge as we wait to vaccinate more of the population. Hopefully we just have a few more months of this before Kansas reaches herd immunity.
Testing
The graph below shows us how Kansas is doing for tests performed (blue line, left y-axis) and the percent of those tests that are positive (red line, right y-axis) on a weekly basis. The goal line for test positivity (5%) is indicated by the gray, dashed line.
GREAT NEWS! Kansas has a test positivity rate that is below the 5% goal line. The challenge is keeping it below 5%. Kansas is ranked #30 in the country for tests performed per 100,000. There was a slight increase in tests reported per 100,000 in the past week for both Kansas and the US.
Cases
The map below comes from the Brown School of Public Health. It grades each county’s level of risk, based on the average daily cases per 100,000 over the most recent 7 days and is current as of Tuesday. Risk is greatest for red counties and least for green counties. Around the beginning of the year, the entire state was red.
Cases are decreasing for all age groups.
The case rate declines for Kansas nearly match the decline for the US. Where case rate has leveled off nationally, case rate continues to decline for Kansas.
Hospitalizations
This week there were 166 newly reported hospital admissions compared to the week prior, a decrease of 11%. The graph below shows us where those hospital admissions are coming from in terms of age group, over the past 8 weeks.
So although hospital admissions declined overall last week, we can see that they’re actually rising for certain age groups, including those 18-54 and 75-84.
There were 59 new ICU admissions in the past week for COVID-19, an increase of 18% compared to the previous week.
Deaths
Using the HHS Community Profile Report (date 03Mar2021), Kansas has the 18th highest newly reported death rate per 100,000 residents in the country.
In the most recent week, Kansas has reported a net increase of 92 deaths, a decrease of 55% compared to the previous week. The graph below shows us how deaths have trended over time, adjusted for each county type’s population size. The statewide average is shown in the black line. You can check your county’s classification here.
The death rate for Kansas has been trending up over the past couple months, however we’ve seen a decrease for the past 2 weeks. The death rate is highest in densely-settled rural counties and lowest in urban counties.
Like cases, deaths are decreasing for every age group. So I’ll save that graph for another time.
We can see how Kansas compares to the national trend for death rate per 100,000 in the graph below. Kansas has seen some really dramatic swings from week to week which may point to problems with timely reporting to the state. Thankfully, the state death rate is nearly equal to the national death rate, but even still, it’s quite a bit higher than before the fall surge began.
That’s it for this week! Enjoy the warmer weather!
References
https://covid.cdc.gov/covid-data-tracker/#vaccinations
https://www.kansasvaccine.gov/
http://www.ipsr.ku.edu/ksdata/ksah/population/popden2.pdf
WHCTF report repository: https://beta.healthdata.gov/Community/COVID-19-State-Profile-Report-Kansas/scin-7ddt
https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/index.html
https://beta.healthdata.gov/National/COVID-19-Community-Profile-Report/gqxm-d9w9
https://beta.healthdata.gov/browse?tags=covid-19-spr
https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2021-02/28-03-01/04-COVID-Oliver.pdf
https://www.census.gov/data-tools/demo/hhp/#/?measures=GVR
Kansas COVID-19 Updates is a free newsletter that depends on reader support. If you wish to subscribe please click the link below. There are free and paid options available.
My Ph.D. is in Medical Microbiology and Immunology. I've worked at places like Creighton University, the Centers for Disease Control & Prevention and Mercer University School of Medicine. All thoughts are my professional opinion and should not be considered medical advice.